What is a gut brain axis
Posted on June 22, 2022
IBS is defined as a gut-brain axis disorder. But what does that actually mean?
What is IBS and what causes it?
Irritable Bowel Syndrome (IBS) is a condition that affects the gut. IBS may cause various symptoms like bloating abdominal pain, excessive gas, diarrhoea or constipation. These symptoms are often brought on if someone eats something they are intolerant or sensitive too. There are many factors that can influence the presentation of these symptoms and although IBS is a physical condition research shows it may be triggered by psychological factors.
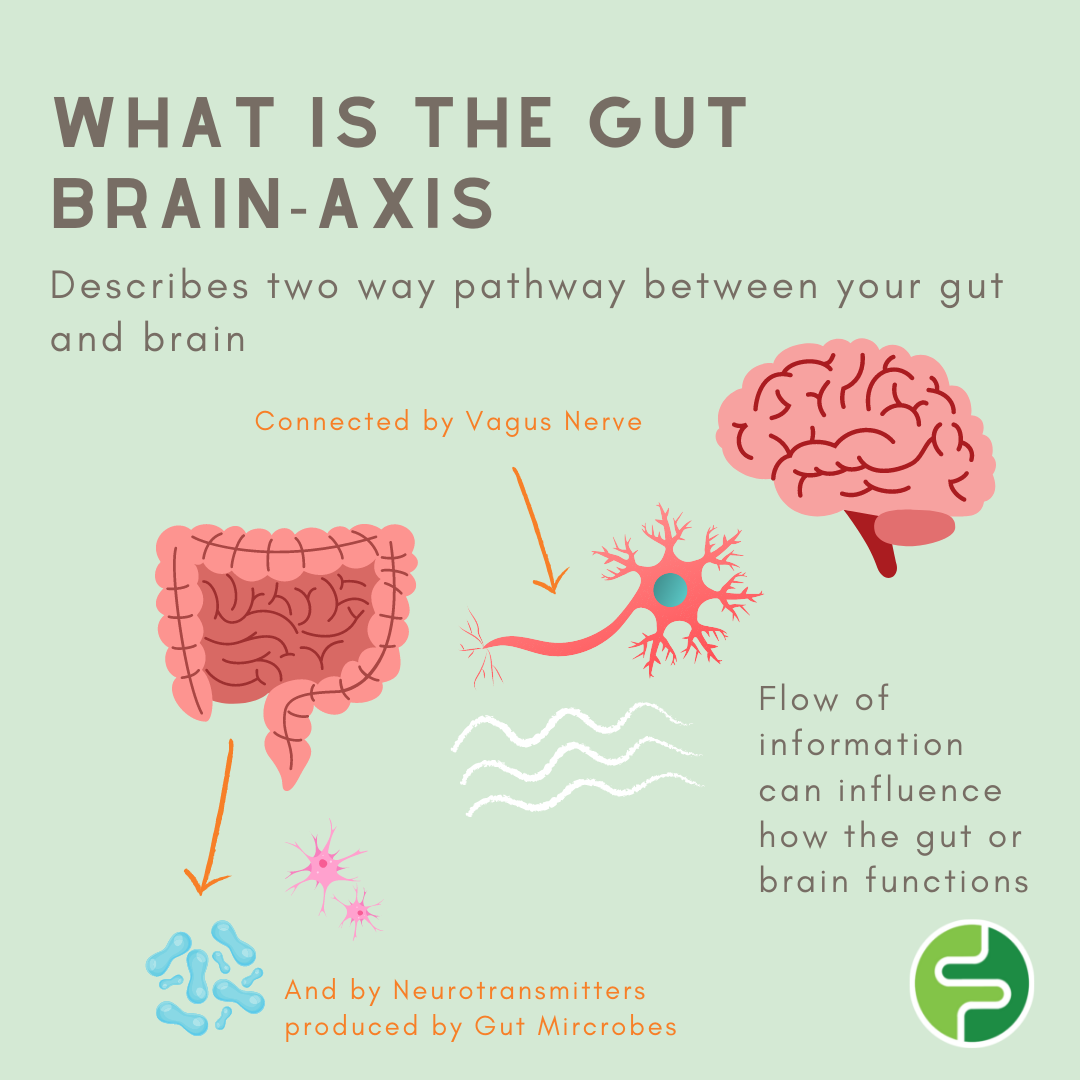
The Gut Brain- axis
The term Gut-Brain axis describes the two way relationship between the gut and the brain. It involves the pathways that connect your enteric nervous system (gut) to your central nervous system (brain). The Vagus nerve connects the two systems and allows the flow of communication between the two. They are also linked through chemical messengers known as neurotransmitters some of which are made by the microbes that live in your gut. These neuro transmitters are used in the brain for many functions including memory and regulation of moods. This flow of information can influence how the gut or brain functions. Brain function can affect digestive function and the health of your gut may affect your mental health.
Guts Microbes – The Key?
Gut Microbes refers to the millions of microorganisms including bacteria that live in your gut. There is emerging evidence that the microbes that live in your gut play a key role in the disturbance of this pathway. An imbalance of this gut bacteria or lack of certain bacteria can affect the signal they are admitting through their neurotransmitters and this may result in incorrect messages to be delivered to the part of the brain responsible for emotion known as the amygdala. This can lead to alteration in mood and mental distress. Multiple studies on IBS patients have found differences in the composition and function of gut microbes compared to healthy individuals and that replacing certain bacteria can help alleviate IBS symptoms.
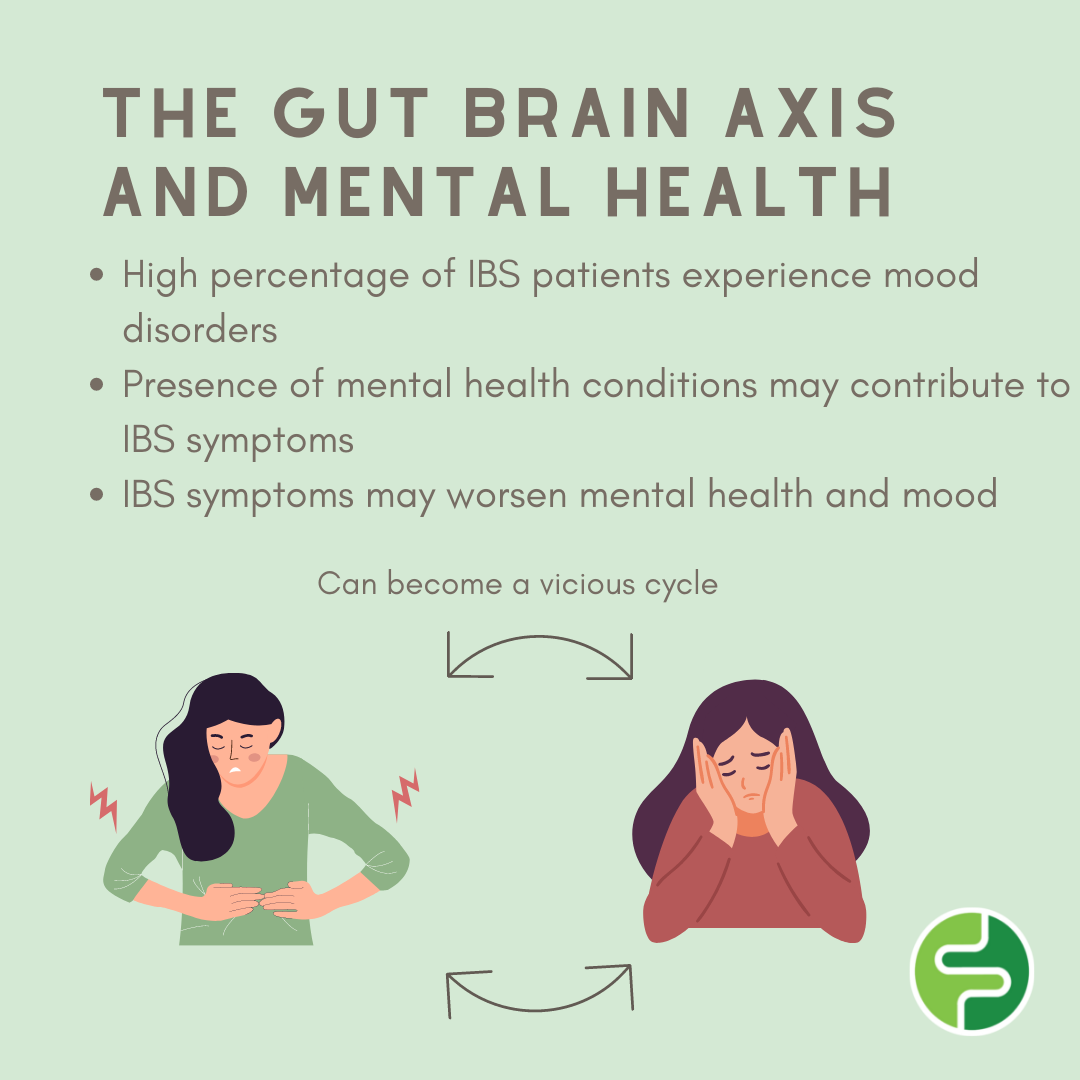
Mental Health, Stress and IBS
A high percentage of IBS patients experience mood disorders or disturbances. The two main mental health conditions associated with IBS are anxiety and depression. As the pathway goes two ways often the presence of these conditions may contribute to IBS symptoms or irritation of the gut may send signals the other way and contribute to the presence of these mental health conditions. Stress is also shown to be a contributing factor to IBS. When we become stressed we release a hormone known as cortisol. This hormone can affect our gut microbe composition and the ability to absorb nutrients. This may lead to heightened gut sensitivity and worsening of IBS symptoms. This can become is vicious cycle as people with IBS may become anxious or stressed about experiencing IBS flare ups, which may then trigger the worsening of IBS symptoms which in turn may increase mental health conditions.
Your gut is ultimately your second brain and can have a profound effect on your quality of life, but there are a number of ways we can manage this pathway to help improve quality of life.
Tips to Improve your Gut-Brain Axis
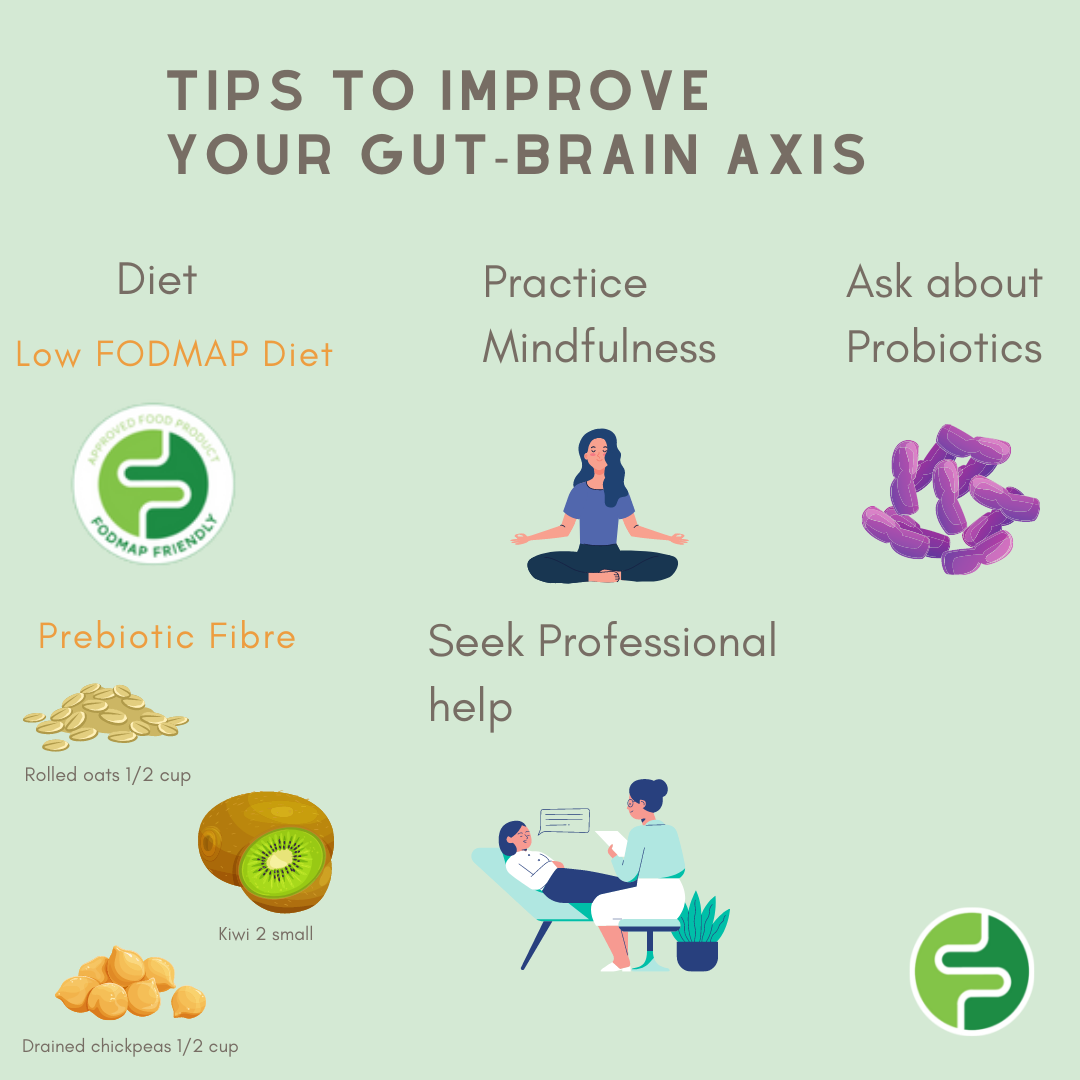
Diet
The right nutrients can stimulate your Vagus nerve to improve its function. Your diet can also effect the composition and function of your gut microbes. Good nutrition can also help with mood and mental health meaning both systems can improve together.
A low FODMAP diet may provide a fast relief from IBS symptoms. Alleviating these symptoms may then in turn help improve mood and mental health. If you have never attempted a low FODMAP diet before this should be done with the supervision of an Accredited Practicing Dietitian. You can also use our FODMAP Friendly App (Android and iOS) to find FODMAP trained Dietitians in your area.
Prebiotic fibre is essential for your gut microbes stay healthy and function correctly. Often prebiotics are high in FODMAPS but can be included in a Low FODMAP diet if serving sizes are appropriate for example a unripe banana, ½ a cup of rolled oats or canned lentils. Use the FODMAP Friendly App to check serving sizes before adding these to your meals.
Talk to a Dietitian about probiotics
Current research shows Probiotics may help alleviate certain symptoms like bloating and abdominal pain in people with IBS. A Dietitian may be able to advise if this is a suitable path for you.
Practice Mindfulness
Practicing mindfulness activities can help with the Gut-brain axis disorder. Activities like deep breathing, meditation, yoga and exercise can help stimulate your Vagus nerve by putting your body into a relaxed state known as the ‘rest and digest’ state. This helps to improve gut function and mood and may ease IBS symptoms.
Seek psychological help when needed
Certain Psychologists are trained in breaking the mind-gut axis that may be worsening IBS symptoms. Psychologists are also a great resource for ongoing support particular when facing difficult times. Talking to your GP start or organisations like Beyond Blue and Headspace are a great place to start or get more information.
Summary
Your gut and brain are connected through the Vagus nerve and neurotransmitters produced by your gut microbe. This pathway may be a major contributing factor to IBS. When this pathway is disturbed or gut microbe balance altered this may trigger IBS symptoms and cause mood disruptions; this can be a viscous cycle. There are ways we can manage this pathway including through good nutrition, using a Low FODMAP diet and by practicing mindfulness activities.