Same, same but different… how do a low FODMAP and Gluten Free diet interact?
Posted on March 10, 2021
A common question we get asked is ‘what is the difference between a low FODMAP and gluten free diet?’ As you’ll see, there are significant similarities, but also nuanced differences between the diets. Today we’re going to do a deep dive into how the low FODMAP, and gluten free diet interact.
Why are gluten free diets sometimes recommended to those with IBS?
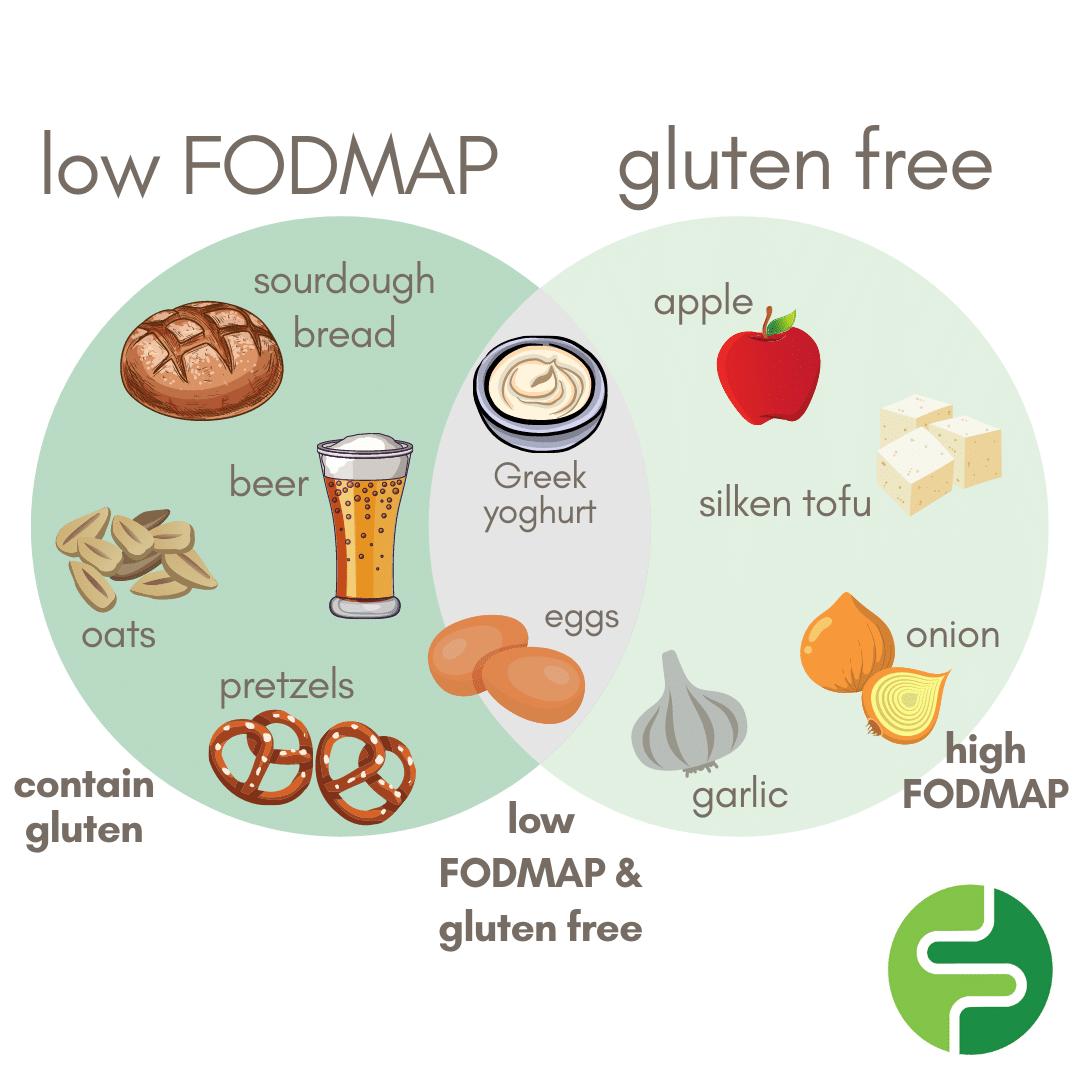
Upon receiving a diagnosis for IBS, a doctor will sometimes recommend the following of a gluten free diet. Why so? Gluten free foods are not necessarily low FODMAP, just as low FODMAP foods are not necessarily gluten free. However, if you imagine a Venn diagram, there is a large ‘grey area’ in the middle of foods that are both low FODMAP and gluten free. Hence, gluten free diets are a good ‘rule of thumb’ recommendation for those with IBS. 
When searching for gluten free foods, there is only one variable to be concerned about – gluten. However, when it comes to FODMAP-containing foods, there are a few more variables to think about. For example, onions may be gluten free, but they are considered high FODMAP – they contain high amounts of fructans (a type of oligosaccharide) and may induce discomfort in those with IBS. This is why it is very important to understand the foods that are gluten free, but high FODMAP in specific quantities.
Gluten free vs. low FODMAP foods – what are the similarities and differences?
A gluten free diet restricts foods containing gluten – namely wheat, barley, rye and triticale. However, gluten is a binding protein, so is added to many processed foods to help give them shape. A gluten free diet will likely restrict the following everyday regular foods:
Most cereal and baking products
Pasta and noodles
Bread, cakes and biscuits
Meat products prepared with breadcrumbs, marinated meats, thickened soups, meat pies
Processed savoury snacks, flavoured potato chips
Alcoholic drinks such as beer, ale and lager

A low FODMAP diet restricts a number of sugars or fermentable carbohydrates known to cause digestive discomfort – namely fructose, lactose, mannitol, sorbitol, GOS and fructans. A range of everyday regular foods that are high in FODMAPS, including but not limited to:
Most cereal and baking products
Bread, cakes and biscuits
Garlic and onions
Fruits such as apples, peaches and plums
Vegetables such as green peas, brussels sprouts and cauliflower
Legumes such as chickpeas and kidney beans
You’ll notice that many of the same foods have been mentioned when describing both the gluten free and low FODMAP diet. Why is this the case? Wheat, barley and rye contain both gluten and FODMAPs – namely fructans, which is a type of oligosaccharide (the ‘O’ in FODMAP). The difference is that the gluten-free diet restricts the protein in these grains, while the low FODMAP diet reduces the carbohydrates in these grains.
What are some hidden high FODMAP ingredients in gluten free foods?
There are a number of ‘hidden’ high FODMAP ingredients that are found in gluten free foods. These include:
Soy:
Soybeans and soy products can be sources of oligosaccharides, especially GOS. However, not all soy products are high FODMAP. Firm tofu is a curd made from soybeans, and the FODMAPs leach into the surrounding liquid, so firm tofu is naturally low in FODMAPs. Note: silken tofu is high FODMAP.
High FODMAP fruits:
The main FODMAP culprits in fruit are sorbitol and fructose. Fruits particularly high in FODMAPs are apples, pears, cherries, figs, pears, watermelon and dried fruit.
Products with garlic and onion:
This unfortunately catches many otherwise low FODMAP gluten free products out. It is important to get into the habit of looking for garlic and onion in the ingredients list of products. Common culprits are pasta sauces, chutneys, packet soups.
Seeds/nuts:
The main FODMAPs present in nuts are GOS and/or fructans. High FODMAP nuts include cashews, almonds and pistachios.
How do I know if I am intolerant to gluten?
There is a difference between a gluten allergy and gluten intolerance. A gluten allergy, also known as Coeliac Disease, is an autoimmune disorder that causes the small intestine lining of genetically susceptible individuals to become damaged every time gluten is consumed. A diagnosis of Celiac Disease is made after a patient tests positive in a coeliac serology (blood) test and a small bowel biopsy. It can only be managed by following a life-long strict gluten free diet. Whereas, gluten intolerance, also known as non-Coeliac gluten sensitivity, has similar symptoms to Coeliac Disease but does not usually cause long-term harm to the body. Someone with gluten intolerance will test negative in a coeliac serology test, so the only way to find out if you are gluten intolerant is by completing the initial phase of low FODMAP diet and seeing if it makes a difference to your symptoms.
It is important to note the process when manufacturers make ‘gluten-free’ products. To extract the protein ‘gluten’, FODMAPs are often removed from the product at the same time. So, people who report being sensitive to gluten and follow the ‘gluten-free’ diet quite often feel better and have symptom improvement due to the lowered FODMAP content, not due to the gluten. This does not apply to those with Coeliac Disease who need to have zero gluten in their diet.
How do I know if I am intolerant to FODMAPs?
Unfortunately, no medical tests currently exist to determine whether you are sensitive to FODMAP carbohydrates. You could look into a hydrogen methane breath test, which is a non-invasive test to identify the presence of fructose, lactose and sorbitol malabsorption as well as proximal small intestine bacterial overgrowth (SIBO). These tests can indicate the extent of malabsorption of fructose, lactose and sorbitol sugars (a monosaccharide, disaccharide and polyol). The test results will provide a good indication of the strictness of dietary restriction required to tailor the diet more specifically to the individual.
The best way to see if FODMAPs are a problem for you is to swap high FODMAP carbohydrates in your diet for low FODMAP foods under the careful supervision of a FODMAP trained Dietitian and see if symptoms improve. However, following a low FODMAP diet is a diagnostic tool, not a forever diet. It is important to remember that the initial low FODMAP phase is designed to set you up to complete the just-as-important ‘challenge’ or reintroduction phase.
What are some examples of low FODMAP, gluten containing foods that I can eat during a gluten challenge?
If you decide to go down the low FODMAP pathway, after following the initial phase of the low FODMAP diet, you’ll want to test out your tolerance to gluten containing foods. Requirements for a gluten challenge will vary depending on the resource you refer to, but the consensus is that around 10g of gluten per day for a six-week period is required to test your tolerance. Check out our blog post dedicated to performing a gluten challenge here.
The importance of consulting a Dietitian when completing the low FODMAP diet
Some high FODMAP foods are highly nutritious foods that our gut bacteria love. In fact, many FODMAPs act like prebiotics and have a positive effect on our gut health. This means restricting all FODMAPs long term could have a negative impact on your gut health and your overall health.
By completing the challenge phase, you will reintroduce FODMAPs and identify which do and do not actually trigger your symptoms. A FODMAP trained Dietitian will help you establish which exact foods trigger your symptoms and what your individual threshold is. Through challenging your thresholds, you may be able to reintroduce some of these beneficial foods and plant diversity back into your diet. This then assists your with personalising your low FODMAP diet on a longer term basis.
In summary
There is a large ‘grey’ area between a low FODMAP and gluten free diet. However, IBS and Coeliac Disease are very different conditions and need to be treated as such.’ For those with IBS, following a gluten free diet means you may still be consuming high FODMAP foods. It is important to consult a Dietitian who will be able to support you in following the low FODMAP diet and referring you to the appropriate health professional as required.
Written by: Charlotte Barber (Student Nutritionist)
Reviewed by: Kiarra Martindale (Accredited Practising Dietitian)