Low FODMAP Vegetarian & Vegan Diets Made Simple with FODMAP Friendly
This week we’re looking at keeping your low FODMAP diet nutritious, delicious and FODMAP Friendly with some top pointers from our expert dietitians.
If you’ve been finding it particularly difficult to find suitable low FODMAP protein, vegetable & legume sources, this blog will be your bible for what you should include in your diet, and what should be moderated*.
What are the nutrients to be looked at when eating a Vegetarian or Vegan Diet?
A vegetarian or vegan diet can be healthy and nutritious when it is planned carefully to ensure all of the essential nutrients are included.
There are several important nutrients that need to be looked at when following a vegetarian or a vegan diet. These include protein, iron, zinc, vitamin B12, calcium and omega-3 fatty acids. In order to achieve adequate intakes of these nutrients, it is suggested to include beans, legumes, nuts, seeds, wholegrains, calcium enriched soy milk and/or alternatives, omega-3 rich foods such as chia seeds and walnuts, into the vegetarian/vegan diet every day.
Let’s refresh: What is a Low FODMAP Diet?
FODMAPs are poorly absorbed short-chain carbohydrates including fructans, galacto-oligosaccharides (GOS), lactose, fructose (in excess of glucose) and polyols. Science based evidence has suggested that a diet low in FODMAPs can alleviate symptoms of Irritable Bowel Syndrome (IBS) in up to 70% of patients (see this blog to learn more).
The low-FODMAP diet isn’t a life-time eating plan. Ideally, with the support of an Accredited Practising Dietitian or a Registered Dietitian, you’ll follow the diet for 2-6 weeks until IBS symptoms settle. Then, you’ll enter the reintroduction phase to identify what subgroups and quantities of FODMAPS you can and can’t tolerate. In the long run, you’ll adhere onto an individualised, modified low FODMAP diet for symptom control by balancing between the restriction of some high FODMAP foods and individual’s food desires as well as nutritional needs.
Combining the Vegetarian or Vegan Diet and the Low FODMAP Diet
It can become very tricky when you are vegetarian or vegan and also need to follow a low FODMAP diet as both diets are restrictive.
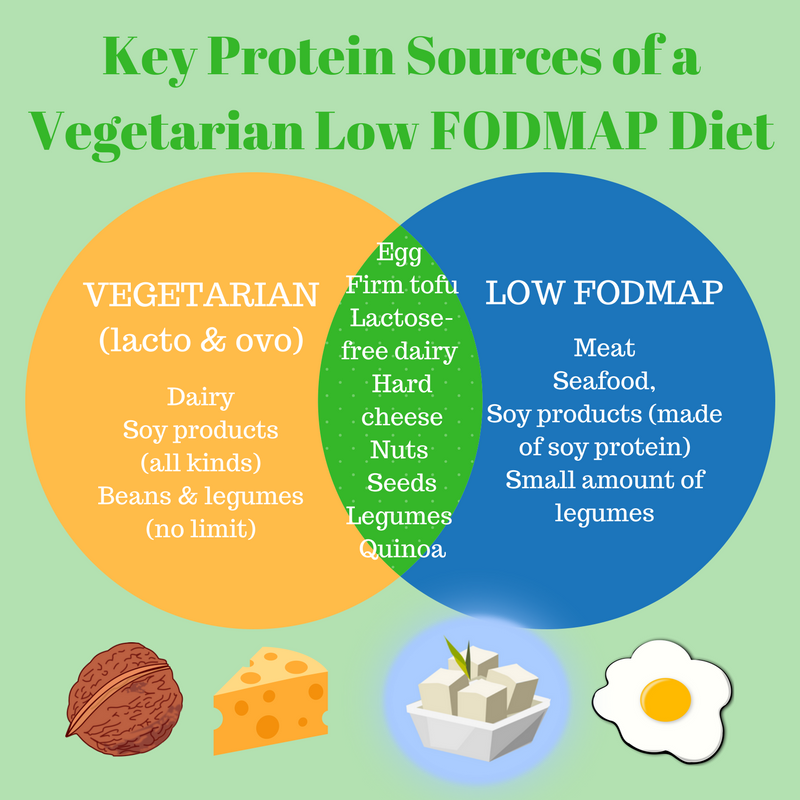
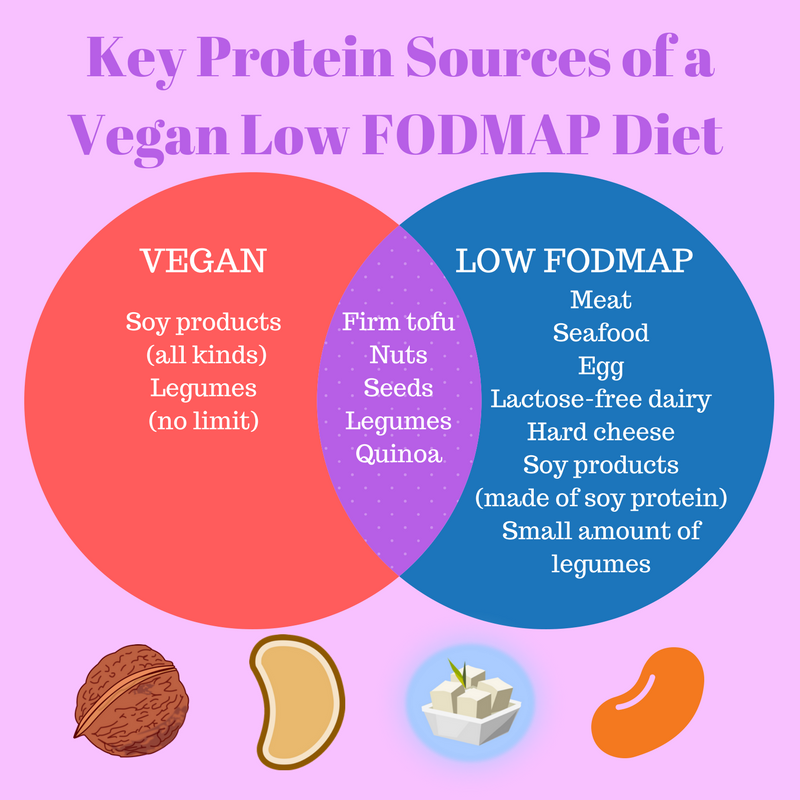
Here are some diagrams showing how protein food sources can be restricted in a vegetarian low FODMAP diet and a vegan low FODMAP diet:
For Vegetarians
For Vegans
The key to achieve a healthy balanced diet is to include a variety of foods from all food groups daily. Although neither of the two diets require you to completely cut out of any of the five core food groups, there is a restriction on the variety of fruits, vegetables/legumes, grains, meat alternatives and dairy products which ultimately might put you at risk of nutritional inadequacy. Therefore, a well-planned diet* is crucial to ensure nutritional adequacy.
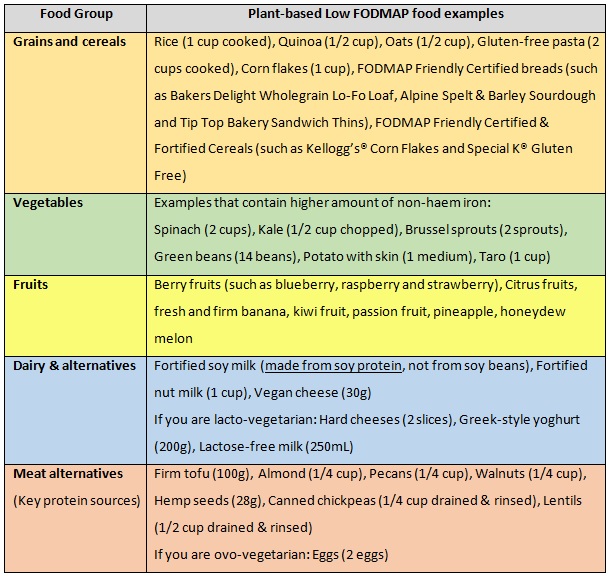
The following table lists some examples in the each of the food groups that adhere to both Vegetarian or Vegan Diets and the Low FODMAP Diet:
You can find all the safe low FODMAP serve sizes of these foods plus many more, in the FODMAP Friendly smartphone App
A few more tips to improve your nutritional intake when following a Vegetarian/Vegan Low FODMAP Diet
Iron is available in two different forms. Non-haem iron comes from plants, and the other form of iron – haem iron – is found only in animal sources, such as red meat. Whilst non-haem iron is less readily absorbed than the haem iron, combining vitamin C-rich foods (such as low FODMAP fruits) with iron-rich foods can help to improve iron absorption.
The FODMAPs in legumes are water-soluble. Drain and rinse your canned legumes (such as chickpeas and lentils) really well before eating them to help reduce the GOS naturally found in them.
A well-planned vegetarian or vegan low FODMAP diet ensures adequate intake of the ‘at risk’ nutrients (protein, iron, zinc, calcium and omega-3 fatty acids). However, vitamin B12 can only be obtained from animal sources. Low FODMAP vegetarians can obtain vitamin B12 from eggs, hard cheese, and lactose-free milk/yoghurt. Vegans, however, are advised to discuss their need for vitamin B12 supplementation with their GP, as this may require close monitoring.
If you are following a vegetarian or vegan low FODMAP diet, it is strongly recommended to seek the support of an Accredited Practising Dietitian or a Registered Dietitian to ensure adequate nutritional intake.
Use the FODMAP Friendly App to Navigate your Low FODMAP Diet
The FODMAP Friendly App helps you identify low FODMAP and high FODMAP plant-based foods. It also contains a list of FODMAP Friendly Certified food products that can be incorporated into your daily diet routine.
Sample day of a healthy plant-based Low FODMAP Diet
BREAKFAST
Vitamin and mineral-fortified low FODMAP breakfast cereal (such as Special K® Gluten Free) with calcium-fortified Almond Milk
½ serve of low FODMAP fruit (such as a kiwi)
MORNING TEA
No-bake cookie (for a single-serve)
Microwave 1 tablespoon of melted almond spread/butter and a drizzle of maple syrup until soft. Then simply combine the melted nut butter mixture with 2 tablespoons of oats and 1 tablespoon of hemp seeds. Shape the mixture into a cookie and pop it in the fridge for 20 minutes to set. Enjoy!
LUNCH
Cheesy pumpkin and spinach sandwich
Alpine Spelt & Sprouted Grains or Alpine Spelt & Barley Sourdough (2 slices), roasted pumpkin (1/2 cup), spinach (1 cup) and vegan cheese (2 slices)
A serve of low FODMAP fruit (such as a clementine)
SNACK
1 pack of Golden Days Original Sesame Snaps or a handful of walnuts/pecans
DINNER
Tofu, chickpea, green bean curry (made with Bay’s Kitchen Jalfrezi Curry Stir-in Sauce) with rice:
Serves 2: Simply sauté tofu cubes (200g), chickpeas (1/2 cup, drained & rinsed), green beans (150g), kale (1 cup chopped), with garlic infused olive oil (such as Cobram Estate Garlic Infused Extra Virgin Olive Oil). Stir in the curry sauce when the ingredients are almost cooked. Leave to simmer for 2 minutes. Serve with rice.
DESSERT
A tub of Coconut Yoghurt (125g), topped with ½ serve of low FODMAP fruit (such as ½ cup of berries)
*Remember that you must consult an Accredited Practising Dietitian (APD) or Registered Dietitian (RD) to receive personalised dietary support. Do not make any changes to your diet without first consulting a healthcare practitioner.
Written by: Flora Cheung (APD, AN)
Edited By: Atlanta Miall-Shorten (APD,AN, AccSD)