Beating unpleasant diarrhoea with your diet
Posted on November 17, 2021
Abdominal cramping? Quick urges to run to the toilet? Poops coming out that resemble gravy or porridge? Diarrhoea can be a pain in the butt, no pun intended.
But what are normal toilet habits and what is diarrhoea?
Most of us have experienced diarrhoea at some points in our lives. Whether it is an acute situation, such as getting the runs post your morning cup of coffee. Or chronic, when the runs usually last more than 2 weeks and may potentially indicate a serious health issue. But what is an ideal poop? The Bristol stool chart (below) indicates what the ideal stool is, types 1 and 2 indicate constipation whereas types 5-7 indicate diarrhoea. Types 3-4 corn on the cob and sausages are the ideal stool. Toilet time should be pain free, strain free, free of cramping, and you should be able to hold on for a short while after feeling the first toilet urges!
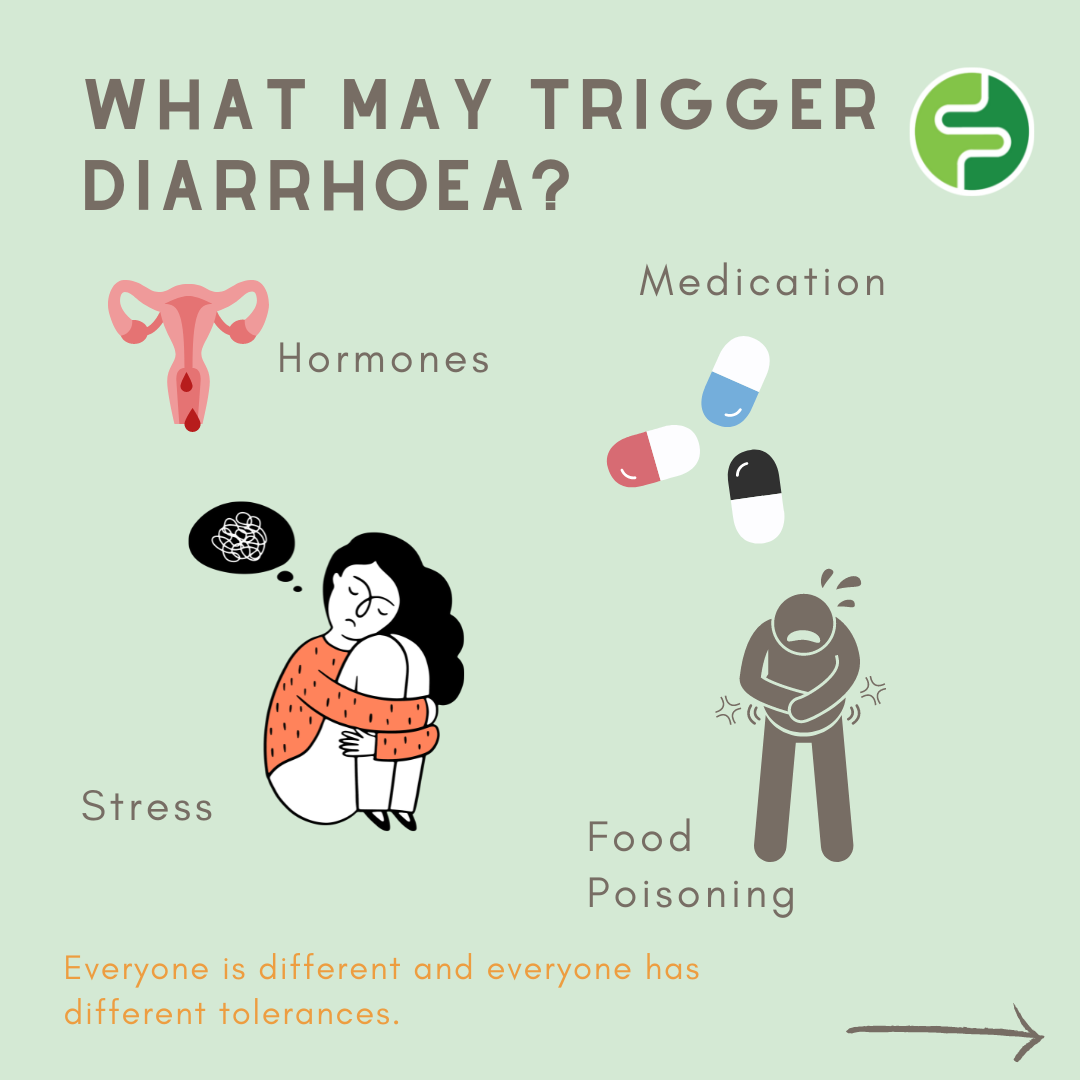
Clinically, diarrhoea is defined as loose watery stools that occur more than 3 times in one day. Diarrhoea may be triggered by a range of factors; illnesses, bacteria that have made their way into the gut, medications, caffeine, alcohol, food intolerances, anxiety or stress, diseases such as coeliac disease and inflammatory bowel disease and for some people; FODMAPs in foods.
Why and how do FODMAPS sometimes cause diarrhoea?
FODMAPs are poorly digested in some individuals and can end up taking a long time to pass through the gut. Certain FODMAPS attract and draw water into the gut whilst they are making their way through the bowel which may result in extra water mixing with your bowel contents resulting in diarrhoea. At the same time gut bacteria feed on these FODMAPs, fermenting them which can produce gas, leading to bloating, cramping and/or abdominal pain. Specifically the water drawing FODMAPs include excess fructose, lactose and the sugar alcohols mannitol and sorbitol.!
How do other foods cause diarrhoea?
Yes, you can have both type one and IBS. Someone with type one diabetes can develop IBS just like anyone else as these conditions are not interrelated and neither cause the other
Certain other nutrients that are renowned for bringing on the runs include; fat, fibre, chilli sugar, dairy, caffeine and alcohol. Fat may cause diarrhoea through malabsorption. Normally fat is absorbed into your blood and doesn’t reach the large intestines, however fat absorption is a complicated process with many steps, and sometimes it doesn’t absorb properly which can lead to oily diarrhoea.
Although fibre has many health benefits, it can exacerbate symptoms of diarrhoea. You may remember that there are two types of fibre; soluble and insoluble. Soluble fibre acts as a bulking agent, it absorbs water and forms a gel. This process slows digestion and the rate of which your gut contents move through your intestine. Insoluble fibre on the other hand draws water into your gut, and stimulates gut movement which increases the movement of your gut contents, and as we already know, water + increased gut movement = diarrhoea.
So how may chilli trigger the runs? As I’m sure you’ve figured out in the past, chillies are hot! You would know this because we have receptors in our mouth that detect the hot chemical ingredient in chillies; capsaicin. We not only have receptors for this chemical in our mouth, but also in our gut. These receptors differ in tolerability between people, some may find chillies fine to consume, whereas others may be more sensitive to capsaicin resulting in increased abdominal discomfort, irritation and increased gut transit time as the food moves through your intestines.
Dairy products contain the FODMAP lactose which is water attracting FODMAPs we spoke about earlier. Caffeine on the other hand, is a stimulant and may accelerate the movement of food through your bowel which can lead to diarrhoea. Alcohol may loosen stools due to a few reasons. 1) Alcohol is usually drunk combined with large amounts of fluid and excess fructose, adding water load to your gut. 2) Alcohol may irritate the lining of your intestine and stimulate speed of digestion. The combination of the fluid and the stimulation can result in cramping, abdominal pain and/or diarrhoea.
What are other reasons for getting diarrhoea?
So why do we sometimes experience diarrhoea when we haven’t eaten at all? There are a few reasons for non-food influences such as stress, hormones, medication, and food poisoning.
Let’s start with bacteria and pathogens. Bacteria and pathogens may make their way into your gut through inhaling them, eating them or through improper hygiene techniques. The majority of your immune system lies in your gut, it is the #1 way for you to “let in” bacteria and pathogens from the outside world, so it makes sense that your body has thought of a pretty good way to get rid of these guys easily. One of these ways is through stimulation of your gut, the bacteria release toxins that are detected by the gut and respond by increasing gut movement to get rid of the pathogens and bacteria, which may result in diarrhoea.
What about stress? The gut is linked to your brain via the gut-brain axis meaning messages are sent from your gut to your brain and your brain to your gut. Have you ever felt the sensation of butterflies in your stomach when you’re nervous or excited? That’s the gut brain axis doing its job. Feelings of stress, anxiety or excitement can send signals to your gut that may speed up gut contractions, and therefore the speed at which food moves through your intestine. Stress may also increase gut permeability (allowing more substances to pass through the gut wall and into the gut). This means more bacteria and pathogens can make their way into your intestines, increasing the likelihood of diarrhoea even more.
Hormones also may play a role in facilitating diarrhoea. Female sex hormones known as prostagladins are released in the luteal phase (days 14-28 of your period, just prior to bleeding). If you’re not pregnant, prostaglandin tells your uterus to shed its lining and facilitate a series of uterus contractions. Prostaglandin may also cause contractions in your intestine which as we know, may quicken the pace of food being pushed through our gut, which may result in diarrhoea. Research has found those with IBS may experience heightened symptoms of cramping, diarrhoea and/or abdominal pain during the luteal phase of their period.
Medications may cause many side effects within the body such as constipation, nausea and/or diarrhoea. Many medications may cause diarrhoea, including; antibiotics, antacids, antidepressants, chemotherapy, anti-inflammatory drugs and the list goes on. Medications all differ in the way they work within the body, therefore the reason they cause diarrhoea depends on how the drug works. It is thought that antibiotics can cause diarrhoea through killing off the good bacteria residing in your gut (as well as the bad bacteria). With some of the good bugs not there to defend the colon, a “bad” bacteria can sometimes survive and produce toxins, stimulating diarrhoea.
Chemotherapy can sometimes destroy the cells lining your intestines that absorb fluid, and may result in extra watery stools.
Laxatives are a well-known medication taken for constipation relief, and can result in loose watery stools as they draw water into the colon and also act as a stimulant, fastening the speed at which the gut moves. There are many other medications with intestinal side effects, and many are still being researched to figure out why they may cause diarrhoea.
How can we combat diarrhoea?
Luckily there are a few things you can do if you are experiencing some of these issues from above. The two things to remember when it comes to diarrhoea, is that diarrhoea is caused mainly by… 1) increased water in the colon, and 2) increased gut movement, your gut speeds up the movement of food through your body.
1. Eat more soluble fibre.
- Remember the two types of fibre mentioned earlier? Insoluble fibre can cause diarrhoea, whereas soluble fibre can help resolve it! Soluble fibre acts like a sponge, and mops up extra water in your gut. This forms a gel-like substance which slows the movement of contents through your gut, and as we know more absorbed water and slower gut transit can reduce diarrhoea.
Foods high in soluble fibre include:
- White bread/pasta
- Rice
- Oats
- Pretzels and crackers
- Cheese and yoghurt
- Smooth peanut butter
- Unfried potato and pumpkin without skins
For more options of low FODMAP foods download the FODMAP Friendly App, available for Apple /iPhones and Android.
Foods to limit (high in insoluble fibre) include:
- Skins, pith, seeds and stems of fruit and vegetables
- Celery
- Mushrooms
- Nuts
- Peas
- Corn
- Raw veggies
- Mango
2. Limit high sugar and high FODMAP foods:
- This differs person to person, everyone has their own tolerability to FODMAPs, and you will need the help of a FODMAP-trained Dietitian to see what foods you are able to tolerate as well as developing a plan to help you wean off this difficult diet.
3. Limit stimulants and gut irritants
- This includes caffeine (again everyone’s tolerance will be different), high fibre foods, alcohol, spicy foods, high fat meals, and foods that you have recognised may bring on the runs. It might be time to give your gut some relief, and limiting these triggering foods could be the answer, if they personally trigger you. Remember, everyone’s tolerance is different.
When to see a doctor?
Apart from being painful and inconvenient, diarrhoea can be dangerous if symptoms last for extended periods. Diarrhoea can cause dehydration through the loss of water and electrolytes through your stools, so it is important to keep up the fluids when experiencing symptoms. Although most cases of diarrhoea will clear up, if diarrhoea lasts more than 2 days, it is best to see your doctor for support.
Other reasons to seek medical advice straight away include:
- Severe abdominal or rectal pain
- Blood in your stool
- Black stools
- Signs of dehydration – dry mouth, confusion, thirst, dizziness, dry skin, fatigue
Dehydration is the most common issue relating to diarrhoea, however it is important to rule out other important health issues that may be an underlying cause for diarrhoea such as:
- Crohn’s disease
- IBD – Inflammatory bowel disease
- IBS – Irritable bowel syndrome
In Summary
Diarrhoea is usually caused by increased fluid to the gut as well as increased gut contractions which may speed up movement of food through your intestines. It is important to find out the triggers and situations which may be triggering your diarrhoea. If symptoms are persisting, see a Dietitian for individualised support.
Written by: Clare Choveaux (Student Dietitian)
Reviewed by: Kiarra Martindale (Accredited Practising Dietitian)