Everything You Need To Know About Irritable Bowel Syndrome (IBS)
Posted on April 01, 2020
It’s IBS Awareness Month this April and we’re kicking it off with a refresher on all things IBS .
For the month of April, the FODMAP Friendly team will be sharing IBS facts, education articles, low FODMAP recipes and answers to your questions each day of this month via our website blog, Facebook, Instagram.
Make sure you follow us on all of our platforms to ensure you don’t miss out on our daily posts.
What is IBS?
IBS is a gastrointestinal disorder where one experiences chronic, relapsing symptoms of constipation, diarrhoea, bloating, abdominal pain, excess and/or excessive wind. These symptoms can be hard to manage and often unpredictable which can have significant flow on effects on everyday activities and quality of life.
IBS is categorised as a functional gastrointestinal disorder (FGD), disorders of gut-brain interaction. FGDs cannot be diagnosed through endoscopy, x-rays or blood tests as there are no structural or biochemical abnormalities in these disorders, hence the term “functional”. Therefore, FGDs including IBS are diagnosed through assessment of symptoms via the ROME IV criteria.
What is the prevalence of IBS?
The prevalence of IBS globally is estimated to be 10-15%, however it is thought that IBS often remains under diagnosed. This is equivalent to around 1 in 7 people globally! About two thirds of those diagnosed with IBS are women.

What causes IBS?
The cause of IBS is not currently well-understood. However, it is known that those with IBS have visceral hypersensitivity in the large intestine. What this means is that those with IBS have extremely sensitive nerve endings in their large intestine. Normal levels of gas production from the digestion of food that would typically be well-tolerated, can induce gastrointestinal symptoms in those with IBS.
Some patients with IBS experience an onset of their first symptoms after gastroenteritis. It is known that enteric infections can lead to damaged nerve endings in the intestine, altering bowel habits and sensitivity levels. This type of IBS is called post infectious IBS (PI-IBS). So this may be one of the causes for IBS however, the vast majority of cases remain unknown.
What are the main symptoms of IBS?
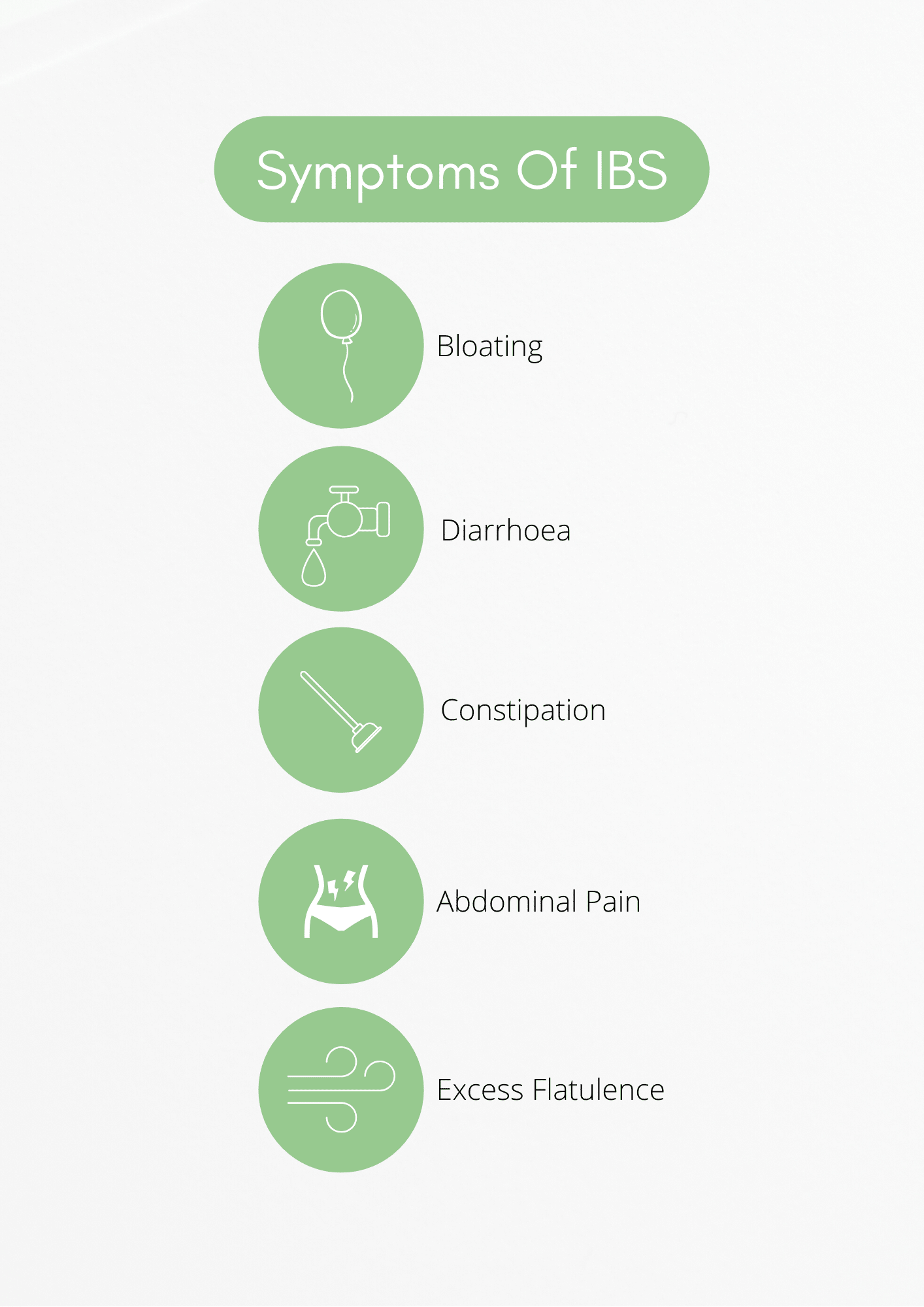
Severity of symptoms often fluctuates depending on a number of factors such as stress, consumption of other dietary triggers, conditions like endometriosis.
There are 4 IBS sub-types encompassing:
- IBS-C – constipation predominant (Scale 1-2 on the Bristol Stool chart)
- IBS-D – diarrhoea dominant (Scale 6-7 on the Bristol Stool chart)
- IBS-M – mixed stool consistency
- IBS-U – unclassified IBS
Reference: Heaton, K W & Lewis, S J 1997, ‘Stool form scale as a useful guide to intestinal transit time’. Scandinavian Journal of Gastroenterology, vol.32, no.9, pp.920 – 924.
How do you diagnose IBS?
The ROME IV criteria is the only method to diagnose IBS. Symptom assessments and diagnosis should only be carried out by your doctor. The diagnostic criteria requires:
- Recurrent abdominal pain 1 day per week associated with two or more of the following:
- Related to defecation
- onset associated with a change in frequency of stool
- onset associated with change in the form of stool
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis.
It is important to speak to your doctor if you believe you may have IBS but have not been diagnosed. Many symptoms of IBS overlap with other medical conditions which are managed very differently, such as Inflammatory bowel disease, Coeliac Disease and Bowel cancers. It is important to rule these conditions out before moving forward with manager IBS.
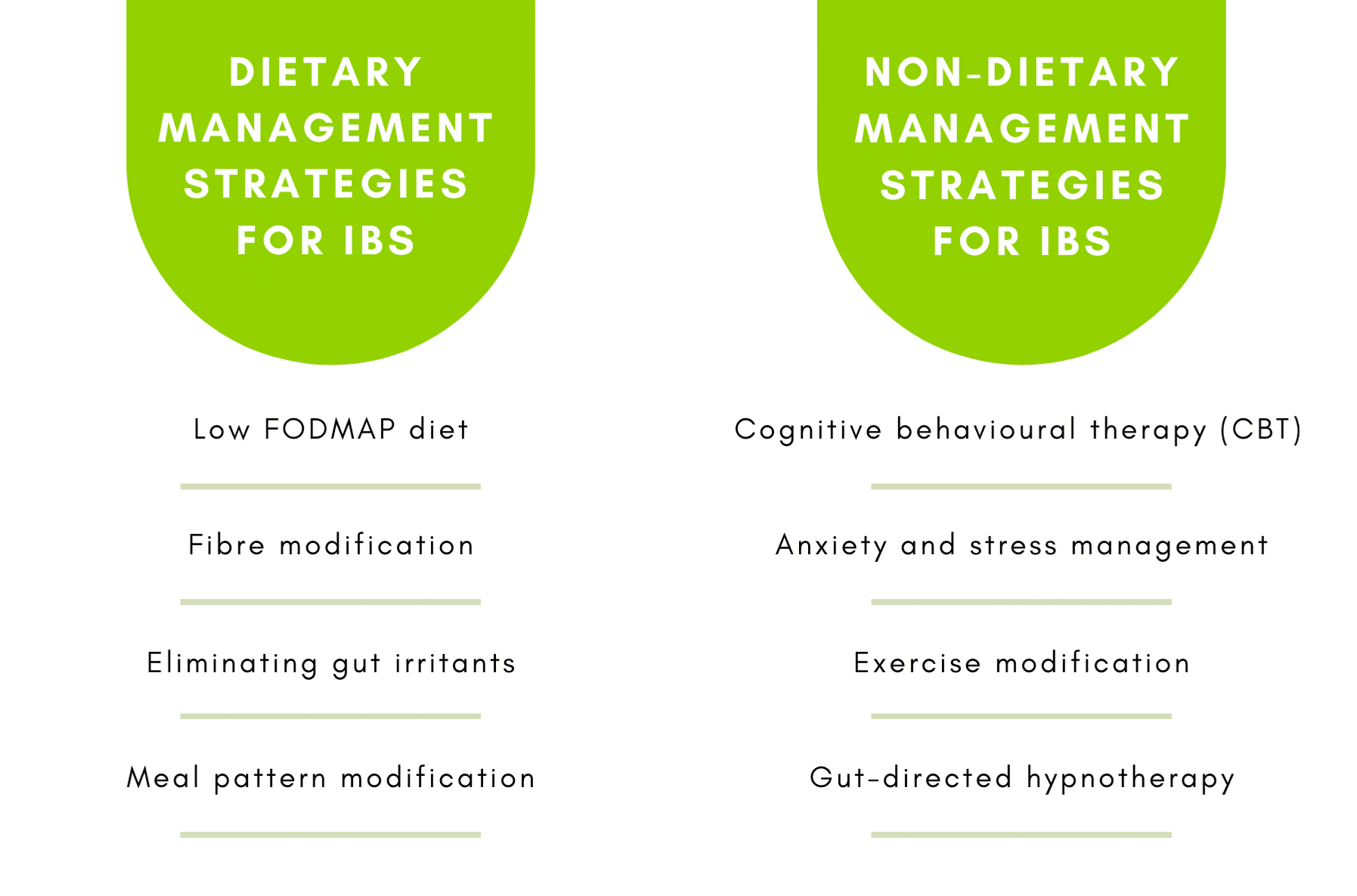
How do you manage IBS?
Unfortunately, there is no cure for IBS. However, there are many management strategies available which can drastically improve the symptoms you are experiencing, including both dietary and lifestyle changes.
What is the Low FODMAP diet?
The Low FODMAP Diet is the most effective diet to manage symptoms of IBS, with up to 75% of people experiencing improvement of symptoms. The low FODMAP diet involved eliminating FODMAPs and tracking symptom improvement, and then challenging each of the FODMAP sugars to determine individual tolerance. The low FODMAP diet is extremely complex and should only be followed under the guidance of a FODMAP trained dietitian.
Tomorrow, we will be sharing a blogpost about the first FODMAP carbohydrate group – oligosaccharides.
Make sure you follow us on our Facebook and Instagram to ensure you don’t miss out on our IBS Awareness posts throughout the month of April.








